Guest blog post by John Gardner and Walter Masalin, Nokia Growth Partners
As obesity and leading a sedentary lifestyle has become more common across the western world, the consequences have started to show at scale. Preventable diseases have become more common, and in fact, the World Health Organization predicts that as much as 20% of the causes of deaths today are attributable to diseases that were either preventable in the first place or could have been managed to prolong life expectancy. More than 400,000 people die each year in the United States as a direct result of obesity and sedentary lifestyle, and perhaps that same amount again is attributable to heart disease, hypertension, and type two diabetes.
Preventative medicine and chronic care management programs have been developed over the years that clinically prove the ability to meaningfully reduce the onset of disease among those at risk, as well as minimize impact and avoid hospitalization or excessive intervention among those who are already experiencing the disease. Yet the impact of these programs has historically been quite small, as morbidity rates continue, and hundreds of billions of dollars are spent each year to manage chronic care for those who develop these diseases.
Changes may be on the horizon, however. Governments, employers and healthcare systems are faced with the fact that they simply cannot afford to cover the costs associated with treating these diseases over such a broad percentage of the population or for such long periods of time. These organizations are investing real dollars into carrot and stick incentive programs in an effort to get patients who are at risk into some preventative care program. Regulatory changes are enabling new services that focus on cost reduction, creating new revenue streams through incentives and mandatory compliance which is pushing the focus to overall health and preventative care. As society starts to embrace the economics behind paying for outcomes versus transactions, incentive program will become more aligned with wellness and preventative measures as well. And, consumers themselves are becoming more empowered to take control of their own health and wellbeing – the concept that, their own behavioural change can be as important a part of managing health as is a visit to the doctor.
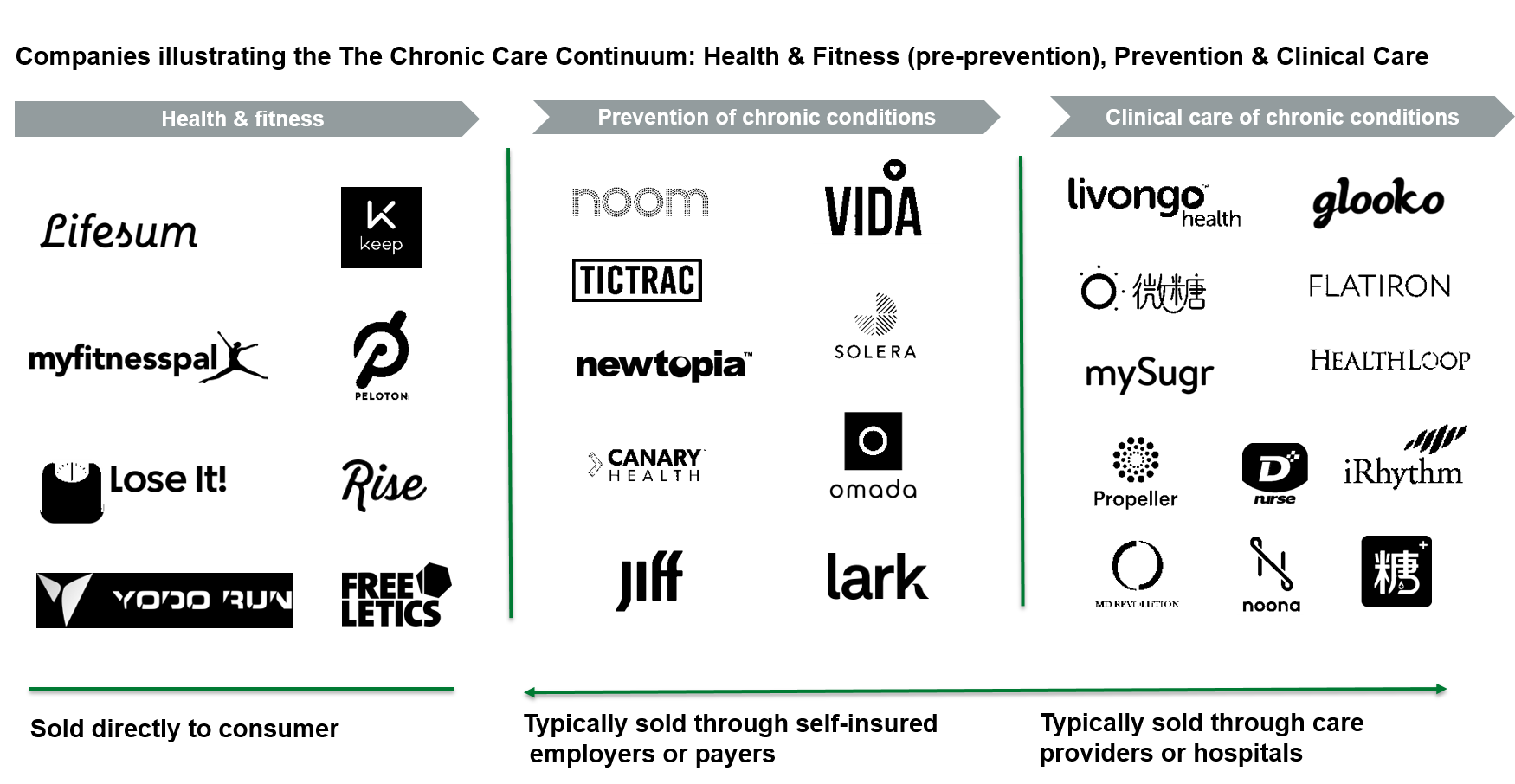
At NGP, we look at the chronic care continuum as having three core categories: health and fitness (pre-prevention), prevention of chronic conditions, and clinical care of chronic diseases. From fitness applications designed to help consumer improve their eating habits or track their achievements, to specific tools to help manage blood sugar or stress levels, to an advanced application that gives offsite access to critical patient information, the next generation of chronic care innovations will be the epicentre of the digital health era.
While the audience and distribution channel, for each chronic care category varies, the success factors for any program remain the same:
- Digital health innovators need to be able to show a demonstrable impact on improved outcomes across a broad sample of the target population;
- Even in the most clinical settings, the program has to be easy to use for the patient/consumer
- Programs need to operate in a way that seamlessly integrates with provider and health system workflows
- Programs need to include meaningful human interaction/coaching in order to sustain engagement over a long period of time
- Programs need to have some measure of positive social re-enforcement in the manner of a classic 12 step program.
At NGP, we are very excited about the ways that entrepreneurs and innovators are leveraging new and cheaper technologies to be able to extend the reach and efficacy of programs, and do so on a scalable basis. Proliferation of low cost sensors, passive collection of increasingly accurate data, cloud based analytics, mobile tools for caregivers, remote patient management, artificial intelligence, tele-care and bot-based compliance re-enforcement- all these recent developments create opportunities to significantly increase the capabilities of new preventative medicine and chronic care management programs. Employer and regulatory driven initiatives are creating the economic pull-thru required to fund outreach and incentivize adoption by the population most in need. We are funding and will continue to fund companies that can impact the outcomes of individuals and populations across the Chronic Care Continuum.
Disclaimer: Chronic Care Continuum landscape visual includes NGP portfolio companies


